Abstract
Introduction:
Patients with malignancies tend to develop a hypercoagulable state which predisposes them to thromboembolic events such as deep vein thrombosis (DVT) and pulmonary emboli (PE). Cancer increases the risk of venous thrombosis several fold with varying degree of relative risks (range 4-7). Various factors including tumor type, location, stage and time since diagnosis influence such incidence. The hospital burden of venous thromboembolism (VTE) associated with cancer has yet to be determined, as well as it's impact on cost, length of stay and mortality. The purpose of this study was to identify the annual trend in incidence, cost, and length of stay of VTE among patients with a diagnosis of cancer as well as determine the associated in-hospital mortality based on cancer origin.
Methods:
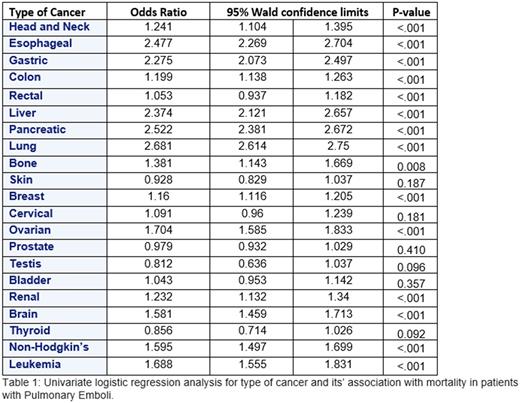
Data on inpatient hospitalizations was collected using the National Inpatient Sample (NIS) for years 2002 to 2014. VTE was identified using the clinical classification software code in conjunction with ICD 9 codes for acute pulmonary embolus. Annual trends for incidence, length of stay, and cost of admission were assessed with a linear regression analysis. Associated cancer type and mortality due to PE was evaluated using univariate logistic regression analysis.
Results:
During the years between 2002 and 2014 a weighted estimate of total admissions for VTE among cancer patients is 903,610. This represents 23% of all admissions for VTE. A trending increase in annual admissions is seen from 61,614 in 2002 to 69,585 in 2014. This increase is primarily driven by a primary diagnosis of acute pulmonary embolus, as these admissions increased from an annual 23,042 to 38,780, while admissions with a primary diagnosis of DVT decreased from 38,571 to 30,805. The total cost of admission increased from $19,380 to $40,105 (p<0.001) while the total length of stay decreased from 6.15 to 4.81 (p<0.001). Mortality among patients with PEs with and without cancer are 2.9% vs 5.6% respectively (p<.0001). Notably, patients with a history of esophageal, gastric, liver, pancreatic and lung cancers all had a more than two-fold increase in the likelihood of mortality.
Conclusion:
Among patients admitted between 2002 and 2014, VTE remains a source of mortality and morbidity, VTE associated with cancer significantly more so. Admissions for VTE are increasing, and this is primarily driven by an increase in acute pulmonary emboli. On the other hand admissions for acute DVT is decreasing which could imply that these are being managed more frequently in the outpatient setting. The mortality from pulmonary emboli doubles with a history of cancer. More specifically mortality in this population is most associated with esophageal, gastric, liver, pancreatic, and lung cancers.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.